kidney
[kid´ne]either of the two bean-shaped organs in the lumbar region that filter the blood, excreting the end-products of body metabolism in the form of urine, and regulating the concentrations of hydrogen, sodium, potassium, phosphate, and other ions in the extracellular fluid.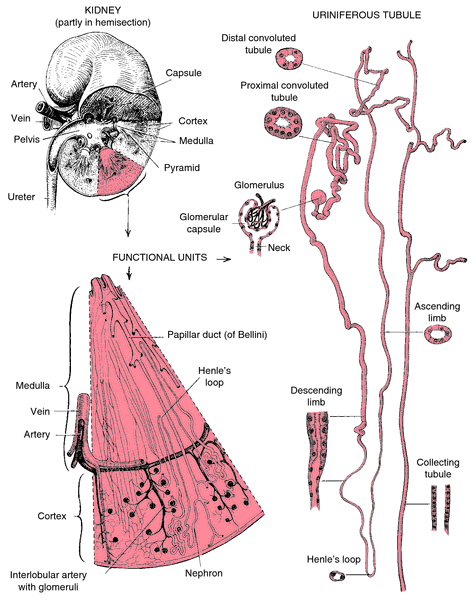
Physiology. In an average adult each kidney is about 10 cm long, 5 cm wide, and 2.5 cm thick, and weighs 120 to 175 g. In this small area the kidney contains over a million microscopic filtering units, the nephrons. Blood arrives at the kidney by way of the renal artery, and is distributed through arterioles into many millions of capillaries which lead into the nephrons. Fluids and dissolved salts in the blood pass through the walls of the capillaries and are collected within the malpighian capsule, the central capsule of each nephron. Within the capsule is a tuft of capillaries called the glomerulus that acts as a semipermeable membrane permitting a protein-free ultrafiltrate of plasma to pass through. This filtrate is forced into the renal tubules, hairpin-shaped collecting channels in the nephrons. Capillaries in the walls of the tubules reabsorb the water and the salts required by the body and deliver them to a system of small kidney veins which, in turn, carry them into the renal vein and return them to the general circulation. Excess water and other waste materials remain in the tubules as urine. The urine contains, besides water, a quantity of urea, uric acid, yellow pigments, amino acids, and trace metals. The urine moves through a system of ducts into the funnel-shaped renal pelvis in each kidney, through which it is led into the two ureters.
Filtering Capacity. About 1500 ml of urine are excreted daily by the average adult. The efficiency of the normal kidney is one of the most remarkable aspects of the body. Ordinarily it draws off from the blood about 164 liters of fluid daily, and usually returns 98 to 99 per cent of the water plus the useful dissolved salts, according to the body's changing needs.
Maintaining Acid-Base Balance. The kidneys help control the body's acidity by reabsorbing filtered bicarbonate ions in exchange for chloride and by secreting hydrogen ions. When there is alkalosis, the kidney compensates by reabsorbing less bicarbonate ions and more hydrogen ions.
Regulation of Sodium-Water Balance. Normal osmolality and volume of body fluids are preserved by the normally functioning kidney. It does this by actively reabsorbing sodium and, by osmosis, reabsorbing more water, thus varying the urine concentration. The regulation of the sodium level in the blood is influenced by aldosterone, which increases sodium reabsorption; it is secreted by the adrenal gland in response to low serum sodium levels and the presence of angiotensin II. The reabsorption of water is affected not only by the reabsorption of sodium but also by antidiuretic hormone, which is secreted by the pituitary gland in response to high serum osmolality.
Endocrine Functions. In response to renal ischemia the kidneys regulate blood pressure by the renin-angiotensin-aldosterone system. Also, when kidney cells become hypoxic they release a hormone called erythropoietin, which stimulates the maturation of oxygen-bearing red blood cells in the bone marrow. The kidneys also are involved in the conversion of inactive vitamin D to the active form, which increases calcium absorption in the intestine and calcium uptake by the bones.
Disorders of the Kidneys. Disorders of the kidney include inflammation, infection, obstruction, structural defects, injuries, calculus formation, and tumors. Specific disorders include types of glomerulonephritis, nephritis, nephropathy, and pyelitis; kidney stones; polycystic kidney disease; and nephroptosis. See also renal failure.
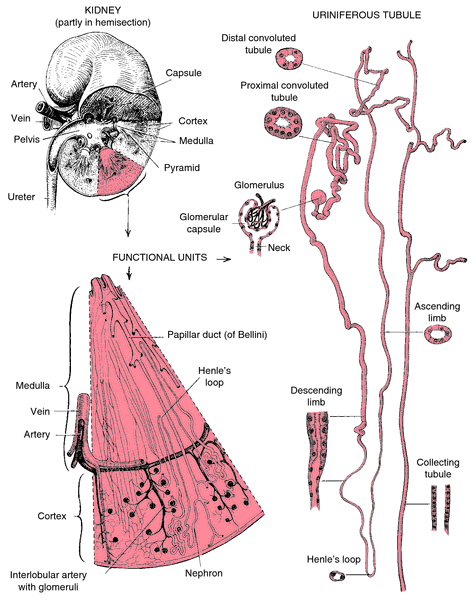
Details of structure of the kidney.
amyloid kidney one with amyloidosis; called also waxy kidney.
artificial kidney popular name for an extracorporeal hemodialyzer, a device used as a substitute for nonfunctioning kidneys.
Ask-Upmark kidney a hypoplastic kidney with fewer lobules than usual and fissures on its surface; most affected persons have severe hypertension, sometimes with hypertensive encephalopathy and retinopathy. The condition may be either congenital or secondary to vesicoureteral reflux with pyelonephritis.
cake kidney a solid, irregularly lobed organ of bizarre shape, formed by fusion of the two renal anlagen; called also lump kidney.
cicatricial kidney a shriveled, irregular, and scarred kidney due to suppurative pyelonephritis.
fatty kidney one with fatty degeneration.
flea-bitten kidney one with small, randomly scattered petechiae on its surface.
floating kidney nephroptosis.
fused kidney a single anomalous organ developed as a result of fusion of the renal anlagen.
horseshoe kidney an anomaly in which the right and left kidneys are linked at one end by a band of tissue as a result of fusion of the poles of the renal anlagen.
hypermobile kidney nephroptosis.
lump kidney cake kidney.
medullary sponge kidney a usually asymptomatic congenital condition in which multiple small cystic dilatations of the collecting tubules of the medullary portion of the renal pyramids give the organ a spongy, porous feeling and appearance. Called also sponge kidney.
myeloma kidney renal changes seen in multiple myeloma, due to filtration of large amounts of Bence Jones protein; they include tubular atrophy with intraluminal casts and multinucleate giant cells in tubular walls and interstitium, resulting in renal failure.
sponge kidney medullary sponge kidney.
kidney stone a calculus in the kidney, composed of crystals precipitated from the urine on a matrix of organic matter. Called also nephrolith and renal calculus.
About 80 per cent of kidney stones are composed of calcium salts, which precipitate out of their normally soluble form in urine, usually because the patient has an inherited tendency to excrete excessive amounts of calcium (idiopathic hypercalcemia). A very small percentage of kidney stones are associated with a parathyroid tumor that increases production of parathyroid hormone and thus raises the serum calcium level. Persons with intestinal absorption problems, including those who have had intestinal bypass surgery for obesity, sometimes develop calcium stones because of excessive absorption of dietary oxalate, which is eventually excreted by the kidneys. Since vitamin C is converted by the body into oxalate, large doses of the vitamin can predispose one to stone formation.
The most common type of stones is the oxalate calculi, hard ones consisting of calcium oxalate; some have sharp spines that can abrade the renal pelvic epithelium, and others are smooth. Another common type is the phosphate calculi, which contain calcium phosphate in a mineral form such as brushite or whitlockite; they may be hard, soft, or friable and range from small to so large that they fill the renal pelvis. Struvite stones are composed of the salt magnesium ammonium phosphate and form in alkaline urine such as that produced in urinary tract infections. Uric acid stones form when there is an increased excretion of uric acid, as in gout or certain malignancies. An acid urine favors their formation. Cystine stones are associated with cystinuria, a hereditary kidney disorder in which there is excessive excretion of cystine. “Staghorn stones” are ones that have extended from the renal pelvis into the calyces, giving them sharp protrusions like the antlers of a stag.
About 80 per cent of kidney stones are composed of calcium salts, which precipitate out of their normally soluble form in urine, usually because the patient has an inherited tendency to excrete excessive amounts of calcium (idiopathic hypercalcemia). A very small percentage of kidney stones are associated with a parathyroid tumor that increases production of parathyroid hormone and thus raises the serum calcium level. Persons with intestinal absorption problems, including those who have had intestinal bypass surgery for obesity, sometimes develop calcium stones because of excessive absorption of dietary oxalate, which is eventually excreted by the kidneys. Since vitamin C is converted by the body into oxalate, large doses of the vitamin can predispose one to stone formation.
The most common type of stones is the oxalate calculi, hard ones consisting of calcium oxalate; some have sharp spines that can abrade the renal pelvic epithelium, and others are smooth. Another common type is the phosphate calculi, which contain calcium phosphate in a mineral form such as brushite or whitlockite; they may be hard, soft, or friable and range from small to so large that they fill the renal pelvis. Struvite stones are composed of the salt magnesium ammonium phosphate and form in alkaline urine such as that produced in urinary tract infections. Uric acid stones form when there is an increased excretion of uric acid, as in gout or certain malignancies. An acid urine favors their formation. Cystine stones are associated with cystinuria, a hereditary kidney disorder in which there is excessive excretion of cystine. “Staghorn stones” are ones that have extended from the renal pelvis into the calyces, giving them sharp protrusions like the antlers of a stag.
Prevention. No matter what the type of kidney stone, an essential preventive measure is high fluid intake to prevent urinary stasis. In order to dilute the urine sufficiently, an adult must put out almost 4000 ml of urine every 24 hours. A continuous flow of adequate amounts of urine has both a mechanical and a chemical effect. The fluids flush the urinary tract and remove substances essential to stone formation. Also, the urine itself contains substances that bind with potential precipitates, making them more soluble and less able to form a mass.
Additional preventive measures include avoidance or prompt treatment of urinary tract infections, changing the urinary pH in cases in which acidity or alkalinity predisposes to stone formation, treatment of underlying pathologies such as parathyroid tumor, and careful long-term follow-up of patients who have had intestinal bypass surgery or a history of intestinal malabsorption.
Uric acid stones can be prevented by administering the drug allopurinol, which inhibits the formation of uric acid, and by keeping the urine relatively alkaline. An alkaline urine and high intake are effective means of preventing cystine stones. If these measures fail, however, the drug penicillamine may be prescribed.
A specific strategy for prevention of stone formation in an individual patient requires chemical analysis of the stones, urine, and blood to determine the type of stone being formed.
Additional preventive measures include avoidance or prompt treatment of urinary tract infections, changing the urinary pH in cases in which acidity or alkalinity predisposes to stone formation, treatment of underlying pathologies such as parathyroid tumor, and careful long-term follow-up of patients who have had intestinal bypass surgery or a history of intestinal malabsorption.
Uric acid stones can be prevented by administering the drug allopurinol, which inhibits the formation of uric acid, and by keeping the urine relatively alkaline. An alkaline urine and high intake are effective means of preventing cystine stones. If these measures fail, however, the drug penicillamine may be prescribed.
A specific strategy for prevention of stone formation in an individual patient requires chemical analysis of the stones, urine, and blood to determine the type of stone being formed.
Symptoms. Kidney stones do not always produce symptoms. However, they can lead to infections and inflammations that do produce symptoms. A definitive diagnosis is established by examination of the urine for hematuria, an abdominal x-ray (which can detect stones of calcium salts), or an intravenous or retrograde pyelogram using a radiopaque dye. The pyelogram will not show the stone itself but there will be a gap in the stream of dye as it courses down the ureter.
The classic symptoms of renal colic occur when a small calculus is dislodged from the renal pelvis and begins to travel down the ureter. Many stones have sharp spicules or spikes on their surfaces; as they roll along the ureter they can scrape the lining, causing excruciating pain and bleeding. The pain is typically felt in the flank over the affected kidney and ureter and radiates downward toward the genitalia and inner thigh. Nausea and vomiting can occur as a result of the severe pain. If an infection is present the patient experiences fever and chills.
The classic symptoms of renal colic occur when a small calculus is dislodged from the renal pelvis and begins to travel down the ureter. Many stones have sharp spicules or spikes on their surfaces; as they roll along the ureter they can scrape the lining, causing excruciating pain and bleeding. The pain is typically felt in the flank over the affected kidney and ureter and radiates downward toward the genitalia and inner thigh. Nausea and vomiting can occur as a result of the severe pain. If an infection is present the patient experiences fever and chills.
Treatment. Stones that are less than 5 mm can usually be eliminated with the normal passage of urine; this is the most desirable method of treatment. Adequate medication is given to relieve pain and relax the muscular walls of the ureter, thus easing passage of the stone. Fluids are given orally or intravenously to aid mechanical flushing. During this period the urine is strained in order to determine whether the stone is passed and, if it is, to collect it for laboratory analysis.
If the stone is not passed, the traditional treatment has been surgical intervention to remove it via ureteroscopy. A newer noninvasive technique is lithotripsy, which involves crushing the stone into fragments small enough to be passed in the urine; this is done using any of a variety of techniques, the most common being ultrasound.
If the stone is not passed, the traditional treatment has been surgical intervention to remove it via ureteroscopy. A newer noninvasive technique is lithotripsy, which involves crushing the stone into fragments small enough to be passed in the urine; this is done using any of a variety of techniques, the most common being ultrasound.
Patient Care. Prevention of kidney stones requires a knowledge of patients most at risk. Males are much more at risk than females for development of calcium stones; also at high risk are those of either sex who have a family history of stone formation. Other persons at risk are those who are immobilized for any reason, have a urinary tract infection, or have a history of intestinal bypass or malabsorption.
Analgesics should be administered promptly to provide relief of pain and facilitate passage of the stone. Fluid intake and output are measured; the intake is encouraged to be 4000 ml every 24 hours. Characteristics of the urine are noted, and all urine is strained until the stone is either passed or removed surgically. Dietary restrictions and recommendations to alter urinary pH and the reason for increased fluid intake are explained to the patient and family members as appropriate. The patient also is taught to take prescribed medications faithfully and to report symptoms of urinary tract infection promptly.
Analgesics should be administered promptly to provide relief of pain and facilitate passage of the stone. Fluid intake and output are measured; the intake is encouraged to be 4000 ml every 24 hours. Characteristics of the urine are noted, and all urine is strained until the stone is either passed or removed surgically. Dietary restrictions and recommendations to alter urinary pH and the reason for increased fluid intake are explained to the patient and family members as appropriate. The patient also is taught to take prescribed medications faithfully and to report symptoms of urinary tract infection promptly.
wandering kidney nephroptosis.
waxy kidney amyloid kidney.
Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
sponge kidney
Polycystic kidney, see there.McGraw-Hill Concise Dictionary of Modern Medicine. © 2002 by The McGraw-Hill Companies, Inc.
Cacchi,
Roberto, Italian physician.Cacchi-Ricci syndrome - Synonym(s): cystic disease of the renal pyramids; medullary polycystic kidney; Ricci-Cacchi syndrome; sponge kidney
Ricci-Cacchi syndrome - Synonym(s): Cacchi-Ricci syndrome
Medical Eponyms © Farlex 2012