Cholecystectomy
Definition
A cholecystectomy is the surgical removal of the gallbladder. The two basic types of this procedure are open cholecystectomy and the laparoscopic approach. It is estimated that the laparoscopic procedure is currently used for approximately 80% of cases.
Purpose
A cholecystectomy is performed to treat cholelithiasis and cholecystitis. In cholelithiasis, gallstones of varying shapes and sizes form from the solid components of bile. The presence of stones, often referred to as gallbladder disease, may produce symptoms of excruciating right upper abdominal pain radiating to the right shoulder. The gallbladder may become the site of acute infection and inflammation, resulting in symptoms of upper right abdominal pain, nausea and vomiting. This condition is referred to as cholecystitis. The surgical removal of the gallbladder can provide relief of these symptoms.
Precautions
Although the laparoscopic procedure requires general anesthesia for about the same length of time as the open procedure, laparoscopy generally produces less postoperative pain, and a shorter recovery period. The laparoscopic procedure would not be preferred in cases where the gallbladder is so inflamed that it could rupture, or when adhesions (additional fibrous bands of tissue) are present.
Description
The laparoscopic cholecystectomy involves the insertion of a long narrow cylindrical tube with a camera on the end, through an approximately 1 cm incision in the abdomen, which allows visualization of the internal organs and projection of this image onto a video monitor. Three smaller incisions allow for insertion of other instruments to perform the surgical procedure. A laser may be used for the incision and cautery (burning unwanted tissue to stop bleeding), in which case the procedure may be called laser laparoscopic cholecystectomy.
In a conventional or open cholecystectomy, the gallbladder is removed through a surgical incision high in the right abdomen, just beneath the ribs. A drain may be inserted to prevent accumulation of fluid at the surgical site.
Preparation
As with any surgical procedure, the patient will be required to sign a consent form after the procedure is explained thoroughly. Food and fluids will be prohibited after midnight before the procedure. Enemas may be ordered to clean out the bowel. If nausea or vomiting are present, a suction tube to empty the stomach may be used, and for laparoscopic procedures, a urinary drainage catheter will also be used to decrease the risk of accidental puncture of the stomach or bladder with insertion of the trocar (a sharp-pointed instrument).
Aftercare
Post-operative care for the patient who has had an open cholecystectomy, as with those who have had any major surgery, involves monitoring of blood pressure, pulse, respiration and temperature. Breathing tends to be shallow because of the effect of anesthesia, and the patient's reluctance to breathe deeply due to the pain caused by the proximity of the incision to the muscles used for respiration. The patient is shown how to support the operative site when breathing deeply and coughing, and given pain medication as necessary. Fluid intake and output is measured, and the operative site is observed for color and amount of wound drainage. Fluids are given intravenously for 24-48 hours, until the patient's diet is gradually advanced as bowel activity resumes. The patient is generally encouraged to walk 8 hours after surgery and discharged from the hospital within three to five days, with return to work approximately four to six weeks after the procedure.
Key terms
Cholecystitis — Infection and inflammation of the gallbladder, causing severe pain and rigidity in the upper right abdomen.
Cholelithiasis — Also known as gallstones, these hard masses are formed in the gallbladder or passages, and can cause severe upper right abdominal pain radiating to the right shoulder, as a result of blocked bile flow.
Gallbladder — A hollow pear-shaped sac on the under surface of the right lobe of the liver. Bile comes to it from the liver, and passes from it to the intestine to aid in digestion.
Care received immediately after laparoscopic cholecystectomy is similar to that of any patient undergoing surgery with general anesthesia. A unique post-operative pain may be experienced in the right shoulder related to pressure from carbon dioxide used through the laparoscopic tubes. This pain may be relieved by laying on the left side with right knee and thigh drawn up to the chest. Walking will also help increase the body's reabsorption of the gas. The patient is usually discharged the day after surgery, and allowed to shower on the second postoperative day. The patient is advised to gradually resume normal activities over a three day period, while avoiding heavy lifting for about 10 days.
Risks
Potential problems associated with open cholecystectomy include respiratory problems related to location of the incision, wound infection, or abscess formation. Possible complications of laparoscopic cholecystectomy include accidental puncture of the bowel or bladder and uncontrolled bleeding. Incomplete reabsorption of the carbon dioxide gas could irritate the muscles used in respiration and cause respiratory distress.
Resources
Other
"Gallstones and Laparoscopic Cholecystectomy." Centers for Disease Control and Prevention. 〈http://www.cdc.gov/nccdphp/ddt/ddthome.htm〉.
"Patient Information Documents on Digestive Diseases." National Institute of Diabetes and Digestive and Kidney Disease. http://www.niddk.nih.gov.
Gale Encyclopedia of Medicine. Copyright 2008 The Gale Group, Inc. All rights reserved.
cholecystectomy
[ko″le-sis-tek´to-me]excision of the gallbladder, usually done to relieve the symptoms of cholecystitis associated with gallstones. During the operation a dye may be injected directly into the biliary ducts and a cholangiogram done to determine whether there are any stones within the ducts. If stones are known or suspected to be in the common bile duct, a T-tube is inserted to bypass the calculi and allow drainage of bile. The end of the tube is brought to the outside through a stab wound in the upper right quadrant and attached to a drainage bag. In spite of the intraoperative cholangiography, some patients will retain stones in the common bile duct after the surgery. laparoscopy is commonly used, which allows most patients to go home on the same day as surgery and return to full activity within a week.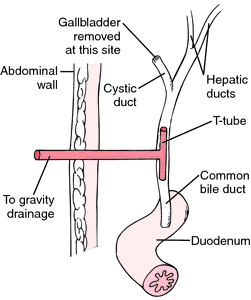
Patient Care. During the preoperative period the patient will be given a thorough physical examination as well as specific tests for liver function and either radiologic or endoscopic studies of the gallbladder and biliary drainage system. Because nausea and flatulence are common problems in these patients, a nasogastric tube usually is inserted and attached to a decompression apparatus prior to surgery.
When the patient returns from surgery a careful check is made for drainage tubes inserted during the operation. Sometimes the drains are devised so that bile and serous fluid from the operative site drain directly onto the surgical dressings. Other drains or tubes such as a T-tube or Y-tube are attached to a drainage bag so that the amount of bile removed can be measured periodically. In either case, dressings over the wound are checked frequently for signs of bleeding or other abnormalities in the character and amount of drainage. When bile leakage is copious, as it sometimes is, the dressings will need to be reinforced and the outer layers changed as often as necessary to keep the patient dry and comfortable and to avoid irritation of the skin around the incision.
The nursing care plan of a patient with either a T-tube or a Y-tube should take into account three major potential problems: infection, obstruction, and dislodgment of the tube. Monitoring for infection includes watching for elevation of body temperature above 100° F and inspection of the tube insertion site for redness, swelling, warmth, and purulent drainage. The patient also is watched for jaundice and complaints of pain in the right upper quadrant, drainage around the tube when it is clamped, nausea, vomiting, and very dark urine and clay-colored stools, all of which indicate obstruction of the common bile duct. The amount of drainage from the tube is measured and recorded at least once every eight hours. A marked decrease in amount could mean that the tube has become dislodged.
Biliary tract disease continues to occur in approximately 5 to 8 per cent of all postcholecystectomy patients. The symptoms can appear within weeks after surgery or may occur years later and are the result of residual stones not removed at the time of surgery, newly formed gallstones, or stricture of the common bile duct. Infections and malignancies also can produce the symptoms of postcholecystectomy syndrome (PCS). Because of hormonal influences, women in the 40- to 49-year-old age group account for almost 80 per cent of patients with PCS. Treatment of the condition varies, but might entail more extensive surgery to provide a means by which bile can drain into the intestines.
When the patient returns from surgery a careful check is made for drainage tubes inserted during the operation. Sometimes the drains are devised so that bile and serous fluid from the operative site drain directly onto the surgical dressings. Other drains or tubes such as a T-tube or Y-tube are attached to a drainage bag so that the amount of bile removed can be measured periodically. In either case, dressings over the wound are checked frequently for signs of bleeding or other abnormalities in the character and amount of drainage. When bile leakage is copious, as it sometimes is, the dressings will need to be reinforced and the outer layers changed as often as necessary to keep the patient dry and comfortable and to avoid irritation of the skin around the incision.
The nursing care plan of a patient with either a T-tube or a Y-tube should take into account three major potential problems: infection, obstruction, and dislodgment of the tube. Monitoring for infection includes watching for elevation of body temperature above 100° F and inspection of the tube insertion site for redness, swelling, warmth, and purulent drainage. The patient also is watched for jaundice and complaints of pain in the right upper quadrant, drainage around the tube when it is clamped, nausea, vomiting, and very dark urine and clay-colored stools, all of which indicate obstruction of the common bile duct. The amount of drainage from the tube is measured and recorded at least once every eight hours. A marked decrease in amount could mean that the tube has become dislodged.
Biliary tract disease continues to occur in approximately 5 to 8 per cent of all postcholecystectomy patients. The symptoms can appear within weeks after surgery or may occur years later and are the result of residual stones not removed at the time of surgery, newly formed gallstones, or stricture of the common bile duct. Infections and malignancies also can produce the symptoms of postcholecystectomy syndrome (PCS). Because of hormonal influences, women in the 40- to 49-year-old age group account for almost 80 per cent of patients with PCS. Treatment of the condition varies, but might entail more extensive surgery to provide a means by which bile can drain into the intestines.
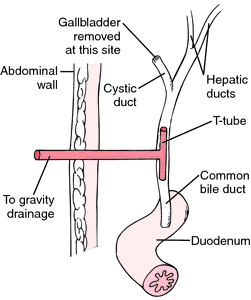
Placement of T-tube following cholecystectomy. From Monahan et al., 1994.
Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
cho·le·cys·tec·to·my
(kō'lē-sis-tek'tō-mē),Surgical removal of the gallbladder.
[chole- + G. kystis, bladder, + ektomē, excision]
Farlex Partner Medical Dictionary © Farlex 2012
cholecystectomy
(kō′lĭ-sĭ-stĕk′tə-mē)n. pl. cholecystecto·mies
Surgical removal of the gallbladder.
The American Heritage® Medical Dictionary Copyright © 2007, 2004 by Houghton Mifflin Company. Published by Houghton Mifflin Company. All rights reserved.
cholecystectomy
Surgery The surgical removal of the gallbladder Indications Gallstones, cholecystitis, cancer. See Bile, Cholecystitis, Gallstones, Laparoscopic cholecystectomy.McGraw-Hill Concise Dictionary of Modern Medicine. © 2002 by The McGraw-Hill Companies, Inc.
cho·le·cys·tec·to·my
(kō'lĕ-sis-tek'tŏ-mē)Surgical removal of the gallbladder.
[chole- + G. kystis, bladder, + ektomē, excision]
Medical Dictionary for the Health Professions and Nursing © Farlex 2012
cholecystectomy
Surgical removal of the gall bladder.Collins Dictionary of Medicine © Robert M. Youngson 2004, 2005
Patient discussion about cholecystectomy
Q. What is a cholecystectomy and how is it done? My Doctor diagnosed me with gallstones and said I have to have a cholecystectomy surgery. What is this and how is it done?
A. Cholecystectomy is a surgery in which the gallbladder is removed. Don't be alarmed since you can live without your gallbladder. When the gallbladder is gone, bile flows directly from the liver into the small intestine.
You will probably have a laparoscopic cholecystectomy, which means a surgeon will make a small slit in your abdomen, then insert a tubelike instrument which has a camera and surgical instruments attached. This is used to take out the gallbladder with the stones inside it.
This procedure causes less pain than open surgery, is less likely to cause complications, and has a faster recovery time. This surgery is performed in an operating room and you will be under general anesthesia. It usually takes 20 minutes to one hour.
You will probably have a laparoscopic cholecystectomy, which means a surgeon will make a small slit in your abdomen, then insert a tubelike instrument which has a camera and surgical instruments attached. This is used to take out the gallbladder with the stones inside it.
This procedure causes less pain than open surgery, is less likely to cause complications, and has a faster recovery time. This surgery is performed in an operating room and you will be under general anesthesia. It usually takes 20 minutes to one hour.
Q. how people deal with after gallbladder removal
A. REMOVE BOTH STONES & GALLBLADDER
More discussions about cholecystectomyThis content is provided by iMedix and is subject to iMedix Terms. The Questions and Answers are not endorsed or recommended and are made available by patients, not doctors.