failure
[fāl´yer]inability to perform or to function properly.
adult failure to thrive a nursing diagnosis accepted by the North American Nursing Diagnosis Association, defined as a progressive functional deterioration of a physical and cognitive nature. The individual's ability to live with multisystem diseases, cope with ensuing problems, and manage his/her care are remarkably diminished.
bone marrow failure failure of the hematopoietic function of the bone marrow; see also bone marrow suppression.
congestive heart failure see congestive heart failure.
heart failure see heart failure.
kidney failure renal failure.
multiple organ failure failure of two or more organ systems in a critically ill patient; see also multiple organ failure.
renal failure see renal failure.
respiratory failure see respiratory failure.
failure to thrive (failure to thrive syndrome) physical and developmental retardation in infants and small children. The syndrome can be seen in children with a physical illness, but the term is most often taken to mean failure to thrive due to psychosocial effects such as maternal deprivation. The syndrome was first noticed when European psychiatrists studied the development of babies who had spent the first five years of their lives in institutions where they were deprived of the emotional warmth of a mother, father, or other primary caregiver.
Characteristics of the failure to thrive syndrome include lack of physical growth (for example, weight and height below the third percentile for age) and below normal achievement in fine and gross motor, social-adaptive, and language skills as assessed by psychometric testing using a tool such as the Denver Developmental Screening Test. Additionally, the child with this syndrome displays withdrawing behavior, avoidance of eye contact, and stiffness or flaccid posture when held. These children often have a history of irritability, feeding problems, and disturbed sleep patterns.
Parents of infants with failure to thrive syndrome typically display feelings of concern and inadequacy. The infant who is feeding poorly and is irritable may elicit a response in the caregiver that reflects tension and frustration. The need for comfort and nurturing by the infant may not be met, and this may lead to a cycle that exacerbates feeding problems.
Intervention encompasses identification of infants and mothers at risk for the syndrome and care of both mother or primary caregiver and infant. The major goals are to encourage the mother to express her feelings without fear of rejection, to model the role of mother and teach her nurturing behaviors, and to promote her self-esteem and confidence. Important nursing goals in the care of the infant include providing optimal nutrition, comfort, and rest; meeting the infant's psychosocial needs; and supplying emotional nurturance and sensory stimulation appropriate to the assessed developmental level.
Characteristics of the failure to thrive syndrome include lack of physical growth (for example, weight and height below the third percentile for age) and below normal achievement in fine and gross motor, social-adaptive, and language skills as assessed by psychometric testing using a tool such as the Denver Developmental Screening Test. Additionally, the child with this syndrome displays withdrawing behavior, avoidance of eye contact, and stiffness or flaccid posture when held. These children often have a history of irritability, feeding problems, and disturbed sleep patterns.
Parents of infants with failure to thrive syndrome typically display feelings of concern and inadequacy. The infant who is feeding poorly and is irritable may elicit a response in the caregiver that reflects tension and frustration. The need for comfort and nurturing by the infant may not be met, and this may lead to a cycle that exacerbates feeding problems.
Intervention encompasses identification of infants and mothers at risk for the syndrome and care of both mother or primary caregiver and infant. The major goals are to encourage the mother to express her feelings without fear of rejection, to model the role of mother and teach her nurturing behaviors, and to promote her self-esteem and confidence. Important nursing goals in the care of the infant include providing optimal nutrition, comfort, and rest; meeting the infant's psychosocial needs; and supplying emotional nurturance and sensory stimulation appropriate to the assessed developmental level.
ventilatory failure respiratory failure.
heart failure
inability of the heart to maintain cardiac output sufficient to meet the body's needs; it most often results from myocardial failure affecting the right or left ventricle.
backward heart failure a concept of heart failure emphasizing the resultant passive engorgement of the systemic venous system that.
congestive heart failure (CHF) that which occurs as a result of impaired pumping capability of the heart that is not keeping up with the metabolic needs of body tissues and organs; it is associated with abnormal retention of water and sodium. It ranges from mild congestion with few symptoms to life-threatening fluid overload and heart failure. Congestive heart failure results in an inadequate supply of blood and oxygen to the body's cells. The decreased cardiac output causes an increase in the blood volume within the vascular system. Congestion within the blood vessels interferes with the movement of body fluids in and out of the various fluid compartments, so that fluid accumulates in the tissue spaces, causing edema.
There are three general kinds of pathologic conditions that can bring about congestive heart failure: (1) ventricular failure, in which the contractions of the ventricles become weak and ineffective, as in myocardial ischemia from coronary artery disease; (2) mechanical failure of the ventricles to fill with blood during the diastole phase of the cardiac cycle, which can occur when the mitral valve is narrowed, as in rheumatic mitral stenosis, or when there is an accumulation of fluid within the pericardial sac (cardiac tamponade) pressing against the ventricles, preventing them from accepting a full load of blood; and (3) an overload of blood in the ventricles during the systole phase of the cycle. High blood pressure, aortic stenosis, and aortic regurgitation are some of the conditions that can cause ventricular overload.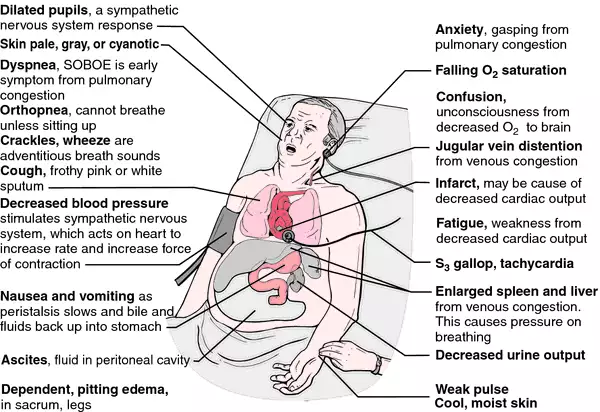
There are three general kinds of pathologic conditions that can bring about congestive heart failure: (1) ventricular failure, in which the contractions of the ventricles become weak and ineffective, as in myocardial ischemia from coronary artery disease; (2) mechanical failure of the ventricles to fill with blood during the diastole phase of the cardiac cycle, which can occur when the mitral valve is narrowed, as in rheumatic mitral stenosis, or when there is an accumulation of fluid within the pericardial sac (cardiac tamponade) pressing against the ventricles, preventing them from accepting a full load of blood; and (3) an overload of blood in the ventricles during the systole phase of the cycle. High blood pressure, aortic stenosis, and aortic regurgitation are some of the conditions that can cause ventricular overload.
Compensatory Mechanisms. In an attempt to compensate for inadequate pumping of the heart, the body uses three basic adaptive mechanisms which, though they are effective for a brief period of time, will eventually become insufficient to meet the oxygen needs of the body. These mechanisms are also responsible for many of the symptoms experienced by the patient with congestive heart failure.
First, the failing heart attempts to maintain a normal output of blood by enlarging its pumping chambers so that they are capable of holding a greater volume of blood. This increases the amount of blood ejected from the heart, but it also leads to fluid overload within the blood vessels and excessive accumulation of body fluids in all of the fluid compartments.
Second, the heart begins to increase its muscle mass in order to strengthen the force of its contractions. This results in ventricular hypertrophy and a need for more oxygen. Eventually, the coronary arteries can no longer meet the oxygen demands of the enlarged myocardium and the patient experiences angina pectoris owing to ischemia.
Third, there is a response from the sympathetic nervous system. The involuntary muscle of the heart is regulated by autonomic, or involuntary, innervation. In response to failing contractility of the myocardial cells, the sympathetic nervous system activates adaptive processes that increase the heart rate, redistribute peripheral blood flow, and retain urine. These mechanisms are responsible for the symptoms of diaphoresis, cool skin, tachycardia, cardiac arrhythmias, and oliguria.
The combined efforts of these three compensatory mechanisms achieve a fairly normal level of cardiac output for a period of time. During this phase of congestive heart failure, the patient is said to have compensated CHF. When these mechanisms are no longer effective the disease progresses to the final stage of impaired heart function and the patient has decompensated CHF.
First, the failing heart attempts to maintain a normal output of blood by enlarging its pumping chambers so that they are capable of holding a greater volume of blood. This increases the amount of blood ejected from the heart, but it also leads to fluid overload within the blood vessels and excessive accumulation of body fluids in all of the fluid compartments.
Second, the heart begins to increase its muscle mass in order to strengthen the force of its contractions. This results in ventricular hypertrophy and a need for more oxygen. Eventually, the coronary arteries can no longer meet the oxygen demands of the enlarged myocardium and the patient experiences angina pectoris owing to ischemia.
Third, there is a response from the sympathetic nervous system. The involuntary muscle of the heart is regulated by autonomic, or involuntary, innervation. In response to failing contractility of the myocardial cells, the sympathetic nervous system activates adaptive processes that increase the heart rate, redistribute peripheral blood flow, and retain urine. These mechanisms are responsible for the symptoms of diaphoresis, cool skin, tachycardia, cardiac arrhythmias, and oliguria.
The combined efforts of these three compensatory mechanisms achieve a fairly normal level of cardiac output for a period of time. During this phase of congestive heart failure, the patient is said to have compensated CHF. When these mechanisms are no longer effective the disease progresses to the final stage of impaired heart function and the patient has decompensated CHF.
Clinical Symptoms. Left-sided heart failure produces dyspnea of varying intensity. In the early stages, shortness of breath occurs only when the patient is physically active. Later, as the heart action becomes more seriously impaired, the dyspnea is present even when the patient is resting. In advanced cases, the patient must sit up in order to breathe (orthopnea). Attacks of breathlessness severe enough to wake the patient frequently occur during sleep (paroxysmal nocturnal dyspnea). These attacks usually are accompanied by coughing and wheezing, and the patient seeks relief by sitting upright. Orthopnea and paroxysmal nocturnal dyspnea are related to congestion of the pulmonary blood vessels and edema of the lung tissues. They are aggravated by lying down because in the prone position quantities of blood in the lower extremities move upward into the blood vessels of the lungs.
Fluid retention is another common symptom of congestive heart failure. In left-sided failure there is higher than normal pressure of blood in the pulmonary vessels. This increased pressure forces fluid out of the intravascular compartment and into the tissue spaces of the lungs, causing pulmonary edema. Right-sided failure causes congestion in the capillaries of the peripheral circulation and results in edema and congestion of the liver, stomach, legs, and feet, and in the sacral region in bedridden patients.
Decreased cardiac output also affects the kidneys by reducing their blood supply, which in turn causes a decrease in the rate of glomerular filtration of plasma from the renal blood vessels into the renal tubules. Sodium and water not excreted in the urine are retained in the vascular system, adding to the blood volume. The diminished blood supply to the kidney also causes it to secrete renin, which indirectly stimulates the secretion of aldosterone from the adrenal gland. Aldosterone in turn acts on the renal tubules, causing them to increase reabsorption of sodium and water, and thus to further increase the volume of body fluids.
Fluid retention is another common symptom of congestive heart failure. In left-sided failure there is higher than normal pressure of blood in the pulmonary vessels. This increased pressure forces fluid out of the intravascular compartment and into the tissue spaces of the lungs, causing pulmonary edema. Right-sided failure causes congestion in the capillaries of the peripheral circulation and results in edema and congestion of the liver, stomach, legs, and feet, and in the sacral region in bedridden patients.
Decreased cardiac output also affects the kidneys by reducing their blood supply, which in turn causes a decrease in the rate of glomerular filtration of plasma from the renal blood vessels into the renal tubules. Sodium and water not excreted in the urine are retained in the vascular system, adding to the blood volume. The diminished blood supply to the kidney also causes it to secrete renin, which indirectly stimulates the secretion of aldosterone from the adrenal gland. Aldosterone in turn acts on the renal tubules, causing them to increase reabsorption of sodium and water, and thus to further increase the volume of body fluids.
Treatment. Medical management of congestive heart failure is aimed at improving contractility of the heart, reducing salt and water retention, and providing rest for the heart muscle. Drugs used to accomplish these goals include digitalis glycosides to slow and strengthen the heartbeat, vasodilators such as nitroprusside and phentolamine to reduce resistance to the flow of blood being pumped from the heart, diuretics to assist in the elimination of water and sodium in the urine, and angiotensin converting enzyme inhibitors to reduce blood pressure, inhibit aldosterone release, and reduce peripheral arterial resistance. beta-blockers are an important adjunct in treatment of heart failure, helping to decrease the sympathetic response. Electroconversion of atrial fibrillation enlists the help of the atria to fill the ventricles to maximum capacity. Biventricular pacing or restoration of cardiac synchrony is helpful for patients with interventricular conduction delay and a wide QRS complex.
Patient Care. Hospitalized patients with severe congestive heart failure present problems related to their needs for physical and mental rest, adequate aeration of the lungs and oxygenation of the tissues, prevention of circulatory stasis, maintenance of the integrity of the skin, restoration and maintenance of fluid and electrolyte balances, and adequate nutrition. The care plan should include frequent monitoring of the vital signs, intake and output, daily weight, serum electrolyte and blood gas levels, and nutritional intake. Patients are placed on sodium-restricted diets and limited fluid intake; they should have a good understanding of the reason for this before leaving the hospital. They should also have a plan for regular exercise as tolerated. Since it is likely that they will continue taking several kinds of medications after returning home, patients or family members should be taught about the pharmacologic action of each drug, the need for taking it exactly as prescribed, any precautions to be taken, and any untoward reactions that warrant notification of the physician, nurse practitioner, or physician's assistant.
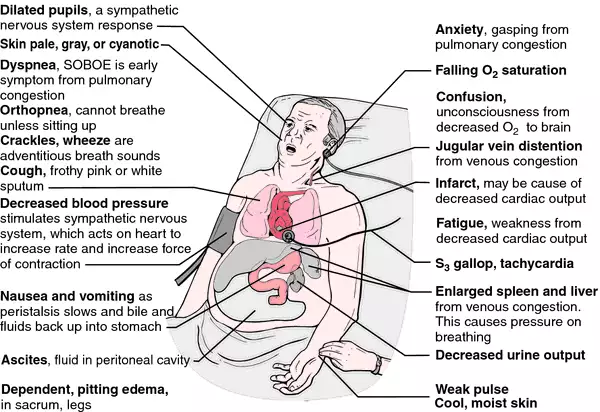
Clinical portrait of congestive heart failure. (SOBOE=shortness of breath on exertion) From Jarvis, 1996.
forward heart failure a concept of heart failure emphasizing the inadequacy of cardiac output as the primary cause.
high-output heart failure that in which cardiac output remains high, associated with conditions such as hyperthyroidism, anemia, and emphysema.
left-sided heart failure (left ventricular heart failure) failure of the left ventricle to maintain a normal output of blood; it does not empty completely and thus cannot accept all the blood returning from the lungs via the pulmonary veins, which become engorged. Fluid seeps out of the veins through the pulmonary capillaries and collects in the interstitial tissue of the lung, causing pulmonary edema that eventually leads to right ventricular heart failure as well.
low-output heart failure that in which cardiac output is diminished, associated with cardiovascular diseases such as coronary artery disease, hypertension, and cardiomyopathy.
right-sided heart failure (right ventricular heart failure) failure of proper functioning of the right ventricle, with subsequent engorgement of the systemic veins, producing pitting edema, enlargement of the liver, and ascites.
Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
heart fail·ure
1. inadequacy of the heart so that as a pump it fails to maintain the circulation of blood, with the result that congestion and edema develop in the tissues;
See also: forward heart failure, backward heart failure, right ventricular failure, left ventricular failure. Synonym(s): cardiac failure, cardiac insufficiency, congestive heart failure, myocardial insufficiency
See also: forward heart failure, backward heart failure, right ventricular failure, left ventricular failure. Synonym(s): cardiac failure, cardiac insufficiency, congestive heart failure, myocardial insufficiency
2. resulting clinical syndromes include shortness of breath, pitting or nonpitting edema, enlarged tender liver, engorged neck veins, and pulmonary rales in various combinations.
Farlex Partner Medical Dictionary © Farlex 2012
congestive heart failure
n.
See heart failure.
The American Heritage® Medical Dictionary Copyright © 2007, 2004 by Houghton Mifflin Company. Published by Houghton Mifflin Company. All rights reserved.
congestive heart failure
Congestive heart disease Cardiology '…a complex clinical syndrome characterized by abnormalities of left ventricular function and neurohormonal regulation, which are accompanied by effort intolerance, fluid retention, and reduced longevity'; an impairment of cardiac function in which failing ventricles cannot adequately perfuse tissue to meet metabolic demands; CHF usually develops over a long period, but may be abrupt in onset Epidemiology CHF is a major health problem which affects 2-3 million, US; 400,000 new cases are diagnosed/yr Clinical Low-output 'forward CHF'–weakness, fatigue, lethargy, light-headedness, and confusion; in decompensated CHF, cardiac cachexia ensues, characterized by exhaustion and loss of lean muscle mass; low-output backward CHF–pulmonary congestion–fluids accumulate in lungs, causing dyspnea, initially only on exertion; also seen, peripheral and pedal edema, rales, S3 gallop, sinus tachycardia, hypotension, ↑ jugular venous pressure, and abdominojugular–hepatojugular reflux High-output heart failure–'non-cardiac' CHF Albright's disease–polyostotic fibrous dysplasia, anemia, carcinoid syndrome, arteriovenous fistulas–trauma, Paget's disease of bone, hemangiomatosis, glomerulonephritis, hemodialysis, liver disease–alcohol-related thiamin deficiency, ↓ peripheral arterial resistance, hyperkinetic heart syndrome, polycythemia vera, thyrotoxicosis CHF precipitants Alcohol, cor pulmonale, drug-related–inappropriate medications, non-compliance, ↑ fluid and/or sodium intake, fever, hypothyroidism, hypoxia, infection, obesity, pregnancy, pulmonary embolism, renal failure, uncontrolled HTN Workup-EKG–to exclude myocardial ischemia or infarction, and/or arrhythmia Workup-lab CBC–to exclude anemia, BUN and creatinine–to assess renal function, electrolytes–K+ and magnesium, liver enzymes, cardiac markers including enzymes–eg, LDH isoenzymes and proteins–e.g., troponin T–to exclude recent MI or ischemia, thyroid function tests–to exclude thyrotoxicosis, a major cause of high-output heart failure Radiology Cardiac enlargement, interstitial and/or alveolar edema, and pulmonary vascular redistribution in acute CHF, findings which are less common in chronic CHF Echocardiography–M-mode, 2-D, & Doppler to determine the left ventricular ejection fraction; CHF typically has concentric left ventricular hypertrophy Management of precipitating factors Eliminate noncardiac factors–eg, alcohol, drugs, excess fluid and/or sodium intake, fever, hypothyroidism, hypoxia, infection, renal insufficiency, HTN, and other factors; control precipitating factors, which may eliminate the signs and symptoms of CHF Acute management Acute CHF with extreme respiratory distress is a medical emergency that requires immediate treatment to ↓ volume–preload and myocardial O2 demand and ↑ forward blood flow Long-term management Once CHF develops, it requires continuous therapy to ↓ M&M–ie,1. non-pharmacologic maneuvers–eg, salt restriction in the form of a 'no salt added' regimen, reduction of alcohol intake, exercise as tolerated and, for Pts with impaired renal function or psychogenic polydipsia, fluid restriction
.
.
2. drug therapy with multiple agents–diuretics, ACE inhibitors, digoxin, nitrates, CCBs, beta-blockers, inotropic agents that ↑ intracellular sodium–eg, vesnarinone–have a narrow therapeutic range Prognosis Poor; 5-yr mortality rate for CHF after the onset of Sx-per Framingham Heart data, is 62% for ♂; 42% for ♀; 200,000 deaths attributable to CHF occur/yr–US; ↑ norepinephrine levels direct correlates with hemodynamic severity and poor prognosis. See Beta-blockers, Calcium channel blockers, Nitrates. .
Congestive heart failure–etiology
Dilated cardiomyopathy Congestive cardiomyopathy
Infectious–eg viral, parasites
Toxic–eg alcohol abuse, adriamycin, cyclophosphamide
Nutritional–eg carnitine, selenium, thiamin, or protein deficiency
Connective tissue disease
Hypertrophic cardiomyopathy Concentric left ventricular hypertrophy
Infiltrative cardiomyopathy Amyloid, hemochromatosis, sarcoidosis
Hypertensive heart disease
Myocardial ischemia/infarction Accompanied by left ventricular dysfunction
Valvular heart disease
McGraw-Hill Concise Dictionary of Modern Medicine. © 2002 by The McGraw-Hill Companies, Inc.
heart fail·ure
(hahrt fāl'yŭr)1. Inadequacy of the heart so that as a pump it fails to maintain the circulation of blood, with the result that congestion and edema develop in the tissues.
See also: forward heart failure, backward heart failure, right ventricular failure, left ventricular failure
Synonym(s): cardiac insufficiency, congestive heart failure, myocardial insufficiency.
See also: forward heart failure, backward heart failure, right ventricular failure, left ventricular failure
Synonym(s): cardiac insufficiency, congestive heart failure, myocardial insufficiency.
2. Resulting clinical syndromes including shortness of breath, pitting edema, enlarged tender liver, engorged neck veins, and pulmonary rales in various combinations.
Medical Dictionary for the Health Professions and Nursing © Farlex 2012
congestive heart failure
See HEART FAILURE.Collins Dictionary of Medicine © Robert M. Youngson 2004, 2005
Congestive heart failure
A condition in which the heart cannot pump enough blood to supply the body's tissues with sufficient oxygen and nutrients; back up of blood in vessels and the lungs causes buildup of fluid (congestion) in the tissues.
Gale Encyclopedia of Medicine. Copyright 2008 The Gale Group, Inc. All rights reserved.
heart fail·ure
(hahrt fāl'yŭr)1. Inadequacy of the heart so that as a pump it fails to maintain the circulation of blood, with the result that congestion and edema develop in the tissues.
2. Resulting clinical syndromes including shortness of breath, pitting edema, enlarged tender liver, and pulmonary rales in various combinations.
Medical Dictionary for the Dental Professions © Farlex 2012
Patient discussion about congestive heart failure
Q. What Is the Treatment for Congestive Heart Failure? My mother is 76 years ols and has been suffering from a heart disease for many years. Lately she has developed congestive heart failure. How is this situation treated?
A. In addition to everything else, she might try CoQ10, a supplement available at most nutrition stores.
"Congestive heart failure has been strongly correlated with significantly low blood and tissue levels of CoQ10 ....
[In numerous studies] treatment with CoQ10 significantly improved heart muscle function while producing no adverse effects or drug interactions."
http://faculty.washington.edu/ely/coenzq10.html
"Congestive heart failure has been strongly correlated with significantly low blood and tissue levels of CoQ10 ....
[In numerous studies] treatment with CoQ10 significantly improved heart muscle function while producing no adverse effects or drug interactions."
http://faculty.washington.edu/ely/coenzq10.html
Q. congestive heart failure how it works is it to do with fluid built up in your body
A. Congestive heart failure (CHF), or heart failure, is a condition in which the heart can't pump enough blood to the body's other organs. The "failing" heart keeps working but not as efficiently as it should. People with heart failure can't exert themselves because they become short of breath and tired.
As blood flow out of the heart slows, blood returning to the heart through the veins backs up, causing congestion in the tissues. Often swelling (edema) results. Most often there's swelling in the legs and ankles, but it can happen in other parts of the body, too. Sometimes fluid collects in the lungs and interferes with breathing, causing shortness of breath, especially when a person is lying down.
Heart failure also affects the kidneys' ability to dispose of sodium and water. The retained water increases the edema.
As blood flow out of the heart slows, blood returning to the heart through the veins backs up, causing congestion in the tissues. Often swelling (edema) results. Most often there's swelling in the legs and ankles, but it can happen in other parts of the body, too. Sometimes fluid collects in the lungs and interferes with breathing, causing shortness of breath, especially when a person is lying down.
Heart failure also affects the kidneys' ability to dispose of sodium and water. The retained water increases the edema.
Q. describe the symptoms of congestive heart failure
A. From my own expierience, EM24 gave an accurate answer. My edema also affects my hands as well as ankles. I was given a Xopenex HFA inhaler to use if lungs are affected.
This content is provided by iMedix and is subject to iMedix Terms. The Questions and Answers are not endorsed or recommended and are made available by patients, not doctors.