jaundice
[jawn´dis]yellowness of skin, sclerae, mucous membranes, and excretions due to hyperbilirubinemia and deposition of bile pigments. It is usually first noticeable in the eyes, although it may come on so gradually that it is not immediately noticed by those in daily contact with the jaundiced person. Called also icterus.
Jaundice is not a disease; it is a symptom of a number of different diseases and disorders of the liver and gallbladder and of hemolytic blood disorders. One such disorder is the presence of a gallstone in the common bile duct, which carries bile from the liver to the intestine. This may obstruct the flow of bile, causing it to accumulate and enter the bloodstream. The obstruction of bile flow may cause bile to enter the urine, making it dark in color, and also decrease the bile in the stool, making it light and clay-colored. This condition requires surgery to remove the gallstone before it causes serious liver injury.
The pigment causing jaundice is called bilirubin. It is derived from hemoglobin that is released when erythrocytes are hemolyzed and therefore is constantly being formed and introduced into the blood as worn-out or defective erythrocytes are destroyed by the body. Normally the liver cells absorb the bilirubin and secrete it along with other bile constituents. If the liver is diseased, or if the flow of bile is obstructed, or if destruction of erythrocytes is excessive, the bilirubin accumulates in the blood and eventually will produce jaundice. Determination of the level of bilirubin in the blood is of value in detecting elevated bilirubin levels at the earliest stages before jaundice appears, when liver disease or hemolytic anemia is suspected.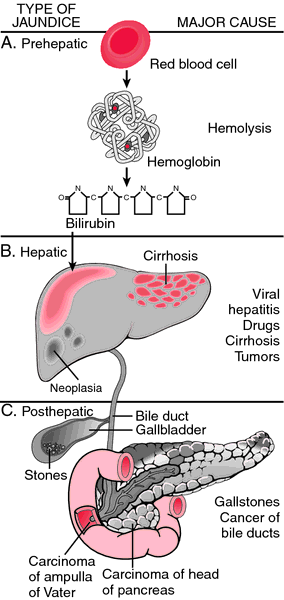
Jaundice is not a disease; it is a symptom of a number of different diseases and disorders of the liver and gallbladder and of hemolytic blood disorders. One such disorder is the presence of a gallstone in the common bile duct, which carries bile from the liver to the intestine. This may obstruct the flow of bile, causing it to accumulate and enter the bloodstream. The obstruction of bile flow may cause bile to enter the urine, making it dark in color, and also decrease the bile in the stool, making it light and clay-colored. This condition requires surgery to remove the gallstone before it causes serious liver injury.
The pigment causing jaundice is called bilirubin. It is derived from hemoglobin that is released when erythrocytes are hemolyzed and therefore is constantly being formed and introduced into the blood as worn-out or defective erythrocytes are destroyed by the body. Normally the liver cells absorb the bilirubin and secrete it along with other bile constituents. If the liver is diseased, or if the flow of bile is obstructed, or if destruction of erythrocytes is excessive, the bilirubin accumulates in the blood and eventually will produce jaundice. Determination of the level of bilirubin in the blood is of value in detecting elevated bilirubin levels at the earliest stages before jaundice appears, when liver disease or hemolytic anemia is suspected.
Patient Care. Assessment of the patient with jaundice includes observations of the degree and location of yellowing, noting the color of urine and stools, and the presence of itching. Since jaundice can be accompanied by severe itching, frequent skin care is important to preserve skin integrity. Tepid sponge baths can help reduce discomfort and promote rest.
Patients with severe jaundice are at risk for encephalopathic changes that produce confusion, impaired mentation, and altered levels of consciousness. The potential for injury is increased and demands vigilance and safety measures to protect the patient.
Patients with severe jaundice are at risk for encephalopathic changes that produce confusion, impaired mentation, and altered levels of consciousness. The potential for injury is increased and demands vigilance and safety measures to protect the patient.
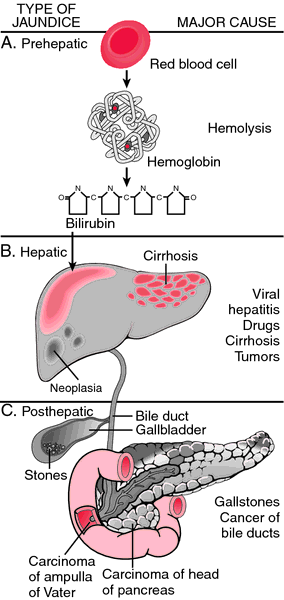
Jaundice may be attributable to prehepatic (A), hepatic (B), or posthepatic (C) causes. From Damjanov, 2000.
acholuric jaundice jaundice without bilirubinemia, associated with elevated unconjugated bilirubin that is not excreted by the kidney. Familial acholuric jaundice is another name for the hereditary form of hemolytic jaundice.
breast milk jaundice elevated unconjugated bilirubin in some breast-fed infants due to the presence of an abnormal pregnane that inhibits glucuronyl transferase conjugating activity.
cholestatic jaundice that resulting from abnormality of bile flow in the liver.
familial nonhemolytic jaundice Gilbert disease.
hematogenous jaundice hemolytic jaundice.
hemolytic jaundice see hemolytic jaundice.
hepatocellular jaundice jaundice caused by injury to or disease of the liver cells.
leptospiral jaundice Weil's syndrome.
neonatal jaundice (jaundice of the newborn) icterus neonatorum.
nonhemolytic jaundice that due to an abnor-mality in bilirubin metabolism.
obstructive jaundice that due to blockage of the flow of bile.
physiologic jaundice mild icterus neonatorum during the first few days after birth.
Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
phys·i·o·log·ic jaun·dice
a form of jaundice observed frequently in newborn infants in the first 1-2 weeks of life. It is caused by several factors, including a comparatively high red blood cell mass at birth compared with that of adults, shorter red blood cell lifespan, transiently impaired conjugation of bilirubin in the liver, and lack of gut flora (which are helpful in intestinal metabolism and excretion of bilirubin); is related to indirect (unconjugated) bilirubinemia that peaks at 2-3 days of age in normal, full-term infants and later with higher levels in preterm infants and is accentuated in breast-fed infants.
Farlex Partner Medical Dictionary © Farlex 2012
neonatal jaundice
Yellowing of a newborn’s skin during the neonatal period, which is caused by an increased bilirubin level in the blood, due to immaturity of liver function plus destruction of red cells. Neonatal jaundice appears between days 2 and 5 and clears by 2 weeks, and is more common in premature infants.DiffDx
Nonphysiologic, prolonged, or pathologic jaundice in newborn, biliary atresia, ABO and/or Rh incompatibility, galactosaemia, cephalhaematoma, polycythemia, G6PD deficiency, neonatal sepsis, congenital infection (CMV), toxoplasmosis, syphilis, herpes, rubella, late-pregnancy use of sulfa drugs by mother, Crigler-Najjar syndrome, hereditary spherocytosis, cystic fibrosis, breast-milk jaundice, pyruvate kinase deficiency, thalassaemia, Gilbert’s syndrome, congenital hypothyroidism, Lucey-Driscoll syndrome, Gaucher’s disease, Niemann-Pick disease.
Segen's Medical Dictionary. © 2012 Farlex, Inc. All rights reserved.
jaundice
Icterus Hepatology A condition characterized by the deposition of excess–> 2 mg/dL, 34 µmol/L free or conjugated BR in peripheral circulation, and in skin, mucosa and sclerae; it is either physiologic–eg, due to hemolysis or pathologic–eg, seen in hepatitis or bile stasis. See Breast milk jaundice, Hyperbilirubinemia, Obstructive jaundice. Jaundice types–unconjugated hyperbilirubinemia
Physiologic jaundice Jaundice develops ≥ 72 hrs after birth; total BR rises to greater than 15 mg/dL; direct BR is < 15% of total BR; jaundice resolves within 1–2 weeks Etiology Sluggish glucuronyl transferase activity, ↑ of BR 'load,' ↓ plasma clearance of BR Management Phototherapy, exchange transfusion
Pathological jaundice Jaundice develops in 72 hrs after birth; total BR peaks at ≤ 15 mg/dL; direct BR is > 15% of total BR; jaundice may require > 2 weeks to resolve Etiology HDN, hemolysis, extravascular loss of blood, ↑ enterohepatic circulation, breast feeding, defective BR metabolism, sepsis, metabolic disease Management Phototherapy, exchange transfusion
McGraw-Hill Concise Dictionary of Modern Medicine. © 2002 by The McGraw-Hill Companies, Inc.
ic·ter·us ne·o·na·to·rum
(ik'tĕr-ŭs nē-ō-nā-tō'rŭm)Jaundice in the newborn; sometimes normal but can be induced or accentuated by excessive hemolysis, sepsis, neonatal hepatitis, or congenital atresia of the biliary system.
Synonym(s): jaundice of the newborn, physiologic icterus, physiologic jaundice.
Synonym(s): jaundice of the newborn, physiologic icterus, physiologic jaundice.
Medical Dictionary for the Health Professions and Nursing © Farlex 2012