Ascites
Definition
Ascites is an abnormal accumulation of fluid in the abdomen.
Description
Rapidly developing (acute) ascites can occur as a complication of trauma, perforated ulcer, appendicitis, or inflammation of the colon or other tube-shaped organ (diverticulitis). This condition can also develop when intestinal fluids, bile, pancreatic juices, or bacteria invade or inflame the smooth, transparent membrane that lines the inside of the abdomen (peritoneum). However, ascites is more often associated with liver disease and other long-lasting (chronic) conditions.
Types of ascites
Cirrhosis, which is responsible for 80% of all instances of ascities in the United States, triggers a series of disease-producing changes that weaken the kidney's ability to excrete sodium in the urine.
Pancreatic ascites develops when a cyst that has thick, fibrous walls (pseudocyst) bursts and permits pancreatic juices to enter the abdominal cavity.
Chylous ascites has a milky appearance caused by lymph that has leaked into the abdominal cavity. Although chylous ascites is sometimes caused by trauma, abdominal surgery, tuberculosis, or another peritoneal infection, it is usually a symptom of lymphoma or some other cancer.
Cancer causes 10% of all instances of ascites in the United States. It is most commonly a consequence of disease that originates in the peritoneum (peritoneal carcinomatosis) or of cancer that spreads (metastasizes) from another part of the body.
Endocrine and renal ascites are rare disorders. Endocrine ascites, sometimes a symptom of an endocrine system disorder, also affects women who are taking fertility drugs. Renal ascites develops when blood levels of albumin dip below normal. Albumin is the major protein in blood plasma. It functions to keep fluid inside the blood vessels.
Causes and symptoms
Causes
The two most important factors in the production of ascites due to chronic liver disease are:
- Low levels of albumin in the blood that cause a change in the pressure necessary to prevent fluid exchange (osmotic pressure). This change in pressure allows fluid to seep out of the blood vessels.
- An increase in the pressure within the branches of the portal vein that run through liver (portal hypertension). Portal hypertension is caused by the scarring that occurs in cirrhosis. Blood that cannot flow through the liver because of the increased pressure leaks into the abdomen and causes ascites.
Other conditions that contribute to ascites development include:
- hepatitis
- heart or kidney failure
- inflammation and fibrous hardening of the sac that contains the heart (constrictive pericarditis)
Persons who have systemic lupus erythematosus but do not have liver disease or portal hypertension occasionally develop ascites. Depressed thyroid activity sometimes causes pronounced ascites, but inflammation of the pancreas (pancreatitis) rarely causes significant accumulations of fluid.
Symptoms
Small amounts of fluid in the abdomen do not usually produce symptoms. Massive accumulations may cause:
- rapid weight gain
- abdominal discomfort and distention
- shortness of breath
- swollen ankles
Diagnosis
Skin stretches tightly across an abdomen that contains large amounts of fluid. The navel bulges or lies flat, and the fluid makes a dull sound when the doctor taps the abdomen. Ascitic fluid may cause the flanks to bulge.
Key terms
Computed tomography scan (CT) — An imaging technique in which cross-sectional x rays of the body are compiled to create a three-dimensional image of the body's internal structures.
Interferon — A protein formed when cells are exposed to a virus. Interferon causes other noninfected cells to develop translation inhibitory protein (TIP). TIP blocks viruses from infecting new cells.
Paracentesis — A procedure in which fluid is drained from a body cavity by means of a catheter placed through an incision in the skin.
Systemic lupus erythematosus — An inflammatory disease that affects many body systems, including the skin, blood vessels, kidneys, and nervous system. It is characterized, in part, by arthritis, skin rash, weakness, and fatigue.
Ultrasonography — A test using sound waves to measure blood flow. Gel is applied to a hand-held transducer that is pressed against the patient's body. Images are displayed on a monitor.
Physical examination generally enables doctors to distinguish ascities from pregnancy, intestinal gas, obesity, or ovarian tunors. Ultrasound or computed tomography scans (CT) can detect even small amounts of fluid. Laboratory analysis of fluid extracted by inserting a needle through the abdominal wall (diagnostic paracentesis) can help identify the cause of the accumulation.
Treatment
Reclining minimizes the amount of salt the kidneys absorb, so treatment generally starts with bed rest and a low-salt diet. Urine-producing drugs (diuretics) may be prescribed if initial treatment is ineffective. The weight and urinary output of patients using diuretics must be carefully monitored for signs of:
- hypovolemia (massive loss of blood or fluid)
- azotemia (abnormally high blood levels of nitrogen-bearing materials)
- potassium imbalance
- high sodium concentration. If the patient consumes more salt than the kidneys excrete, increased doses of diuretics should be prescribed
Moderate-to-severe accumulations of fluid are treated by draining large amounts of fluid (large-volume paracentesis) from the patient's abdomen. This procedure is safer than diuretic therapy. It causes fewer complications and requires a shorter hospital stay.
Large-volume paracentesis is also the preferred treatment for massive ascites. Diuretics are sometimes used to prevent new fluid accumulations, and the procedure may be repeated periodically.
Alternative treatment
Dietary alterations, focused on reducing salt intake, should be a part of the treatment. In less severe cases, herbal diuretics like dandelion (Taraxacum officinale) can help eliminate excess fluid and provide potassium. Potassium-rich foods like low-fat yogurt, mackerel, cantaloupe, and baked potatoes help balance excess sodium intake.
Prognosis
The prognosis depends upon the condition that is causing the ascites. Carcinomatous ascites has a very bad prognosis. However, salt restriction and diuretics can control ascites caused by liver disease in many cases.
Therapy should also be directed towards the underlying disease that produces the ascites. Cirrhosis should be treated by abstinence from alcohol and appropriate diet. The new interferon agents maybe helpful in treating chronic hepatitis.
Prevention
Modifying or restricting use of salt can prevent most cases of recurrent ascites.
Resources
Books
Berkow, Robert, editor. The Merck Manual of Medical Information. Whitehouse Station, NJ: Merck Research Laboratories, 1997.
Organizations
American Liver Foundation. 1425 Pompton Ave., Cedar Grove, NJ 07009. (800) 223-0179. http://www.liverfoundation.org.
Other
"Hepatic and Liver Disorders." The Meck Page. April 20, 1998. http://www.merck.com.
Gale Encyclopedia of Medicine. Copyright 2008 The Gale Group, Inc. All rights reserved.
ascites
[ah-si´tēz]abnormal accumulation of serous fluid (edema) within the peritoneal cavity. It may be associated with any of numerous disorders, including neoplastic and inflammatory disorders of the peritoneum that produce increased permeability of the peritoneal capillaries; severe hypoalbuminemia from any cause; portal hypertension associated with cirrhosis of the liver, advanced congestive heart failure, and constrictive pericarditis; and hyperaldosteronism with increased retention of sodium and water. adj., adj ascit´ic.
In portal hypertension there is increased pressure within the sinusoids and hepatic veins. As the pressure increases there is movement of protein-rich plasma filtrate into the hepatic lymphatics. Some of the fluid enters the thoracic duct, but if the pressure is high enough, the excess fluid will ooze from the surface of the liver into the peritoneal cavity. Because the fluid has a high colloidal osmotic pressure owing to its high protein content, it is not readily reabsorbed from the peritoneal cavity.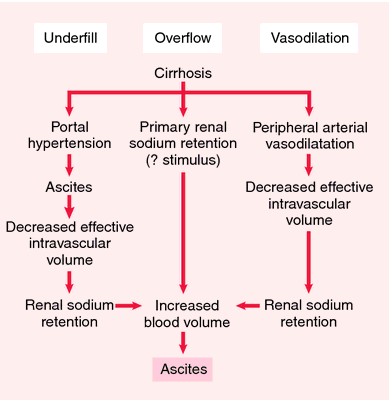
 (see accompanying illustration), recording daily weight gain and loss, and determining the extent to which pressure from the fluid is interfering with respiration, circulation, and digestion. Most patients with ascites are more comfortable in high Fowler's position. When a change of position is necessary to maintain integrity of the skin and promote circulation, small pillows can be used to support the rib cage while the patient is lying on the side. Ascites is usually a chronic condition that is difficult to control. Management must include instruction to the patient and significant others, particularly the caregivers who will help with home care.
(see accompanying illustration), recording daily weight gain and loss, and determining the extent to which pressure from the fluid is interfering with respiration, circulation, and digestion. Most patients with ascites are more comfortable in high Fowler's position. When a change of position is necessary to maintain integrity of the skin and promote circulation, small pillows can be used to support the rib cage while the patient is lying on the side. Ascites is usually a chronic condition that is difficult to control. Management must include instruction to the patient and significant others, particularly the caregivers who will help with home care.
In portal hypertension there is increased pressure within the sinusoids and hepatic veins. As the pressure increases there is movement of protein-rich plasma filtrate into the hepatic lymphatics. Some of the fluid enters the thoracic duct, but if the pressure is high enough, the excess fluid will ooze from the surface of the liver into the peritoneal cavity. Because the fluid has a high colloidal osmotic pressure owing to its high protein content, it is not readily reabsorbed from the peritoneal cavity.
Treatment. Because ascites is symptomatic of an underlying disorder that can range from liver failure to endocrine disease, treatment of the primary disorder is a major goal. The problems of fluid and electrolyte imbalance that are associated with ascites, and the potential for mechanical trauma due to pressure against internal organs adjacent to the abdominal cavity necessitate some kind of symptomatic relief.
Medical treatment includes restriction of fluid and sodium intake and administration of diuretics. Supplementation of potassium and chloride may be necessary during diuretic therapy to avoid an imbalance of these electrolytes. Careful measurement of intake and output is essential, and laboratory values for the electrolytes must be monitored frequently.
Surgical treatment was at one time almost entirely limited to abdominal paracentesis for removal of large accumulations of ascitic fluid. It is, however, only a temporary measure that poses problems of rapid fluid shift, loss of protein, and the potential for introducing infectious agents into the peritoneum. A more effective procedure is the insertion of a peritoneovenous shunt (LeVeen shunt), which provides a means for continuous reinfusion of ascitic fluid into the venous system.
Medical treatment includes restriction of fluid and sodium intake and administration of diuretics. Supplementation of potassium and chloride may be necessary during diuretic therapy to avoid an imbalance of these electrolytes. Careful measurement of intake and output is essential, and laboratory values for the electrolytes must be monitored frequently.
Surgical treatment was at one time almost entirely limited to abdominal paracentesis for removal of large accumulations of ascitic fluid. It is, however, only a temporary measure that poses problems of rapid fluid shift, loss of protein, and the potential for introducing infectious agents into the peritoneum. A more effective procedure is the insertion of a peritoneovenous shunt (LeVeen shunt), which provides a means for continuous reinfusion of ascitic fluid into the venous system.
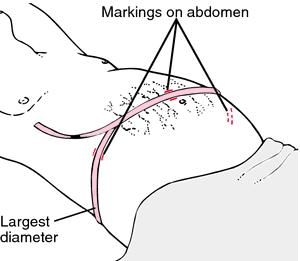
Patient Care. Assessment of the degree of fluid accumulation and the problems it presents to the patient can be done by measuring abdominal girth
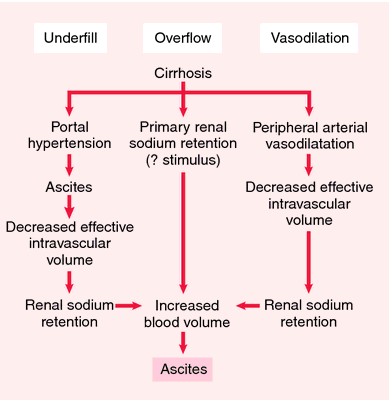
Pathogenesis of ascites: different theories. Three important factors in the production of ascites in cirrhosis are portal hypertension, hypoalbuminemia, and hepatic blockage of lymphatic flow with local overproduction. From Aspinall and Taylor-Robinson, 2001.
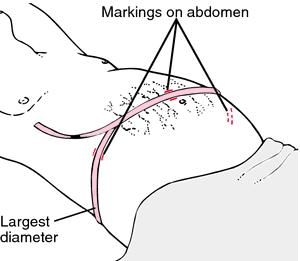
How to measure abdominal girth of a patient with ascites. With patient supine, the tape measure is brought around the largest diameter of the abdomen and a measurement is taken. Before the tape is removed, the abdomen is marked along the sides of the tape on the flanks (sides) and midline to ensure that later measurements are taken in a consistent manner. Redrawn from Ignatavicius and Workman, 2002.
Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
as·ci·tes
(ă-sī'tēz),Accumulation of serous fluid in the peritoneal cavity.
[L. fr. G. askos, a bag, + -ites]
Farlex Partner Medical Dictionary © Farlex 2012
ascites
(ə-sī′tēz)n. pl. ascites
An abnormal accumulation of serous fluid in the abdominal cavity.
as·cit′ic (-sĭt′ĭk) adj.
The American Heritage® Medical Dictionary Copyright © 2007, 2004 by Houghton Mifflin Company. Published by Houghton Mifflin Company. All rights reserved.
ascites
The pathological accumulation of serous fluid in the peritoneal (abdominal) cavity, which common in the decompensated (advanced) liver disease and develops in 50% of those with cirrhosis; patients with cirrhosis who develop ascites have a 50% 2-year survival.Clinical findings
Abdominal distension which, if extreme, causes shortness of breath, portal hypertension and water and Na+ retention.
Aetiology
• Liver—Cirrhosis, alcoholic hepatitis, massive metastases to liver, fulminant hepatic failure, vascular compromise (cardiac failure), Budd-Chiari syndrome, portal vein thrombosis, veno-occlusive disease, fatty liver of pregnancy.
• Extrahepatic—Peritoneal carcinomatosis, peritoneal TB, biliary or pancreatic ascites, nephrotic syndrome, serosal inflammation.
Lab
Hypoalbuminaemia, specific gravity < 1.010, protein content of ≤ 3%.
Management
Paracentesis, decreased Na+ in diet, diuretics, liver transplant, peritoneal shunt, transjugular intrahepatic portosystemic shunt (TIPS), extracorporeal ultrafiltration and reinfusion.
Vox populi
Water in the abdomen.
Segen's Medical Dictionary. © 2012 Farlex, Inc. All rights reserved.
ascites
GI disease A pathologic accumulation of serous fluid in the peritoneal–abdominal cavity, common in decompensated–advanced–liver disease, that develops in 50% of those with cirrhosis; Pts with cirrhosis who develop ascites have a 50% 2-yr survival Etiology-hepatic Cirrhosis, alcoholic hepatitis, massive metastases to liver, fulminant hepatic failure, vascular compromise–cardiac failure, Budd-Chiari syndrome, portal vein thrombosis, veno-occlusive disease, fatty liver of pregnancy extrahepatic origin Peritoneal carcinomatosis, peritoneal TB, biliary or pancreatic ascites, nephrotic syndrome, serosal inflammation Clinical Abdominal distension which, if extreme, causes SOB, portal HTN, water and Na+ retention Lab Hypoalbuminemia, specific gravity < 1.010, protein content of ≤ 3% Treatment Paracentesis, ↓ Na+ in diet, diuretics, liver transplant, peritoneal shunt, transjugular intrahepatic portosystemic shunt–TIPS, extracorporeal ultrafiltration and reinfusion. See Dialysis ascites, Malignant ascites.McGraw-Hill Concise Dictionary of Modern Medicine. © 2002 by The McGraw-Hill Companies, Inc.
as·ci·tes
(ă-sī'tēz)Accumulation of serous fluid in the peritoneal cavity. May be a complication of cirrhosis, congestive heart failure, malignancy, or peritonitis.
Synonym(s): hydroperitoneum, hydroperitonia.
Synonym(s): hydroperitoneum, hydroperitonia.
[L. fr. G. askos, a bag, + -ites]
Medical Dictionary for the Health Professions and Nursing © Farlex 2012
ascites
A collection of fluid in the peritoneal cavity-the space in the ABDOMEN surrounding the internal organs. Ascites occurs in HEART FAILURE, the NEPHROTIC SYNDROME and in CIRRHOSIS of the LIVER.Collins Dictionary of Medicine © Robert M. Youngson 2004, 2005
as·ci·tes
(ă-sī'tēz)Accumulation of serous fluid in the peritoneal cavity.
[L. fr. G. askos, a bag, + -ites]
Medical Dictionary for the Dental Professions © Farlex 2012
Patient discussion about ascites
Q. Does ascites mean it's the end? My mother, age 65 was diagnosed with ovarian cancer in a routine US examination. It was also diagnosed she already has mild ascites. Does that mean her cancer is metastatic?
A. Ascites can render the staging of the cancer as metastatic, but it depends on the specific characters of the ascites, so further testing is needed here.
More discussions about ascitesThis content is provided by iMedix and is subject to iMedix Terms. The Questions and Answers are not endorsed or recommended and are made available by patients, not doctors.