tamponade
[tam″po-nād´]1. surgical use of a tampon.
2. pathologic compression of a part.
cardiac tamponade compression of the heart due to collection of fluid or blood in the pericardium. It may be either chronic or acute. Chronic cardiac tamponade occurs when fluid slowly enters the pericardial sac, allowing time for the membrane's expansion to accommodate the fluid, which can be as much as 1 liter. This gradual filling may or may not produce changes in cardiac hemodynamics. However, if there is rapid filling of the pericardial sac, as little as 200 ml can precipitate a life-threatening emergency. The ultimate effect of cardiac tamponade is reduced cardiac output and inadequate tissue perfusion.
Causes of acute cardiac tamponade include pericarditis with effusion of serosanguineous fluid into the sac, and either surgical or accidental trauma with leakage of blood into the sac. Occasionally, anticoagulant therapy can lead to extensive bleeding around the heart and cardiac tamponade.
Excessive fluid within the pericardial sac causes pressure against the cardiac structures, interferes with ventricular and atrial filling, and compromises blood supply to the myocardium via the coronary vessels. These conditions occur because of the following events: The compressed atria cannot fill as they normally would and so less blood is available for the ventricles; thus preload (the volume of blood in the ventricles at the end of diastole) is reduced. Ventricular filling is further impaired by compression of the ventricles. As pressure within the ventricles rises because of tamponade, pressure differences between the atria and ventricles are reduced, causing the valves between the two chambers to close before the ventricles have had time to fill completely. Increasing pressure within the heart chambers and in the pericardium impinges on the coronary arteries and veins, reducing blood supply to the myocardium, slowing contractility, and further reducing cardiac output.
Clinical features of cardiac tamponade include increased central venous pressure, falling arterial blood pressure, tachycardia, faint or muffled heart sounds, a narrowing pulse pressure, and an exaggerated inspiratory fall in systolic blood pressure (pulsus paradoxus). Hypoxia of cerebral tissues can produce confusion, restlessness, agitation, panic, and a sense of impending doom. Peripheral hypoxia is signaled by changes in the color, temperature, and excessive sweating.
Diagnosis can be confirmed by echocardiography and other radiologic studies. However, if the situation is acute, these tests cannot be done without endangering the life of the patient; thus diagnosis must be based on clinical findings. Once tamponade is suspected, fluids are administered and a pericardiocentesis is done to remove the compressing fluid.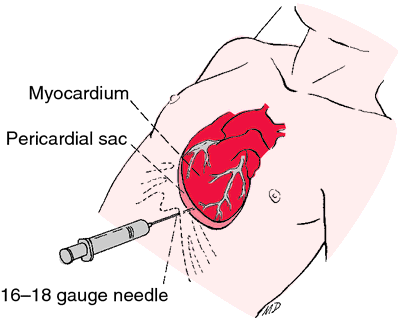
Causes of acute cardiac tamponade include pericarditis with effusion of serosanguineous fluid into the sac, and either surgical or accidental trauma with leakage of blood into the sac. Occasionally, anticoagulant therapy can lead to extensive bleeding around the heart and cardiac tamponade.
Excessive fluid within the pericardial sac causes pressure against the cardiac structures, interferes with ventricular and atrial filling, and compromises blood supply to the myocardium via the coronary vessels. These conditions occur because of the following events: The compressed atria cannot fill as they normally would and so less blood is available for the ventricles; thus preload (the volume of blood in the ventricles at the end of diastole) is reduced. Ventricular filling is further impaired by compression of the ventricles. As pressure within the ventricles rises because of tamponade, pressure differences between the atria and ventricles are reduced, causing the valves between the two chambers to close before the ventricles have had time to fill completely. Increasing pressure within the heart chambers and in the pericardium impinges on the coronary arteries and veins, reducing blood supply to the myocardium, slowing contractility, and further reducing cardiac output.
Clinical features of cardiac tamponade include increased central venous pressure, falling arterial blood pressure, tachycardia, faint or muffled heart sounds, a narrowing pulse pressure, and an exaggerated inspiratory fall in systolic blood pressure (pulsus paradoxus). Hypoxia of cerebral tissues can produce confusion, restlessness, agitation, panic, and a sense of impending doom. Peripheral hypoxia is signaled by changes in the color, temperature, and excessive sweating.
Diagnosis can be confirmed by echocardiography and other radiologic studies. However, if the situation is acute, these tests cannot be done without endangering the life of the patient; thus diagnosis must be based on clinical findings. Once tamponade is suspected, fluids are administered and a pericardiocentesis is done to remove the compressing fluid.
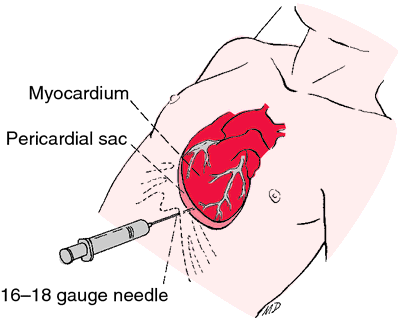
Pericardiocentesis is performed to remove compressing fluid in cardiac tamponade. From Polaski and Tatro, 1996.
Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
tam·po·nade
, tamponage (tam'pŏ-nād', tam'pŏ-nij), Avoid the mispronunciation tam-pō-nahd'.1. Pathologic compression of an organ.
2. Synonym(s): tamponing
Farlex Partner Medical Dictionary © Farlex 2012
tamponade
Cardiology See Balloon tamponade Medtalk A pathologic plugging of an organ–eg, cardiac tamponade, caused by massive accumulation of pericardial fluid, resulting in a mechanical limitation of organ function. See Cardiac tamponade.McGraw-Hill Concise Dictionary of Modern Medicine. © 2002 by The McGraw-Hill Companies, Inc.
tam·pon·ade
, tamponage (tam'pŏ-nād', -nazh')1. Pathologic compression of a joint.
2. The insertion of a tampon.
Medical Dictionary for the Health Professions and Nursing © Farlex 2012
tamponade
Obstruction to the blood flow to or through and organ by external pressure. The term is applied most commonly to compression of the heart, usually from a collection of fluid in the pericardial sac, as in PERICARDITIS or cardiac injury. This prevents normal heart filling and leads to breathlessness and sometimes collapse from reduced heart output. Fluid can be withdrawn through a needle.Collins Dictionary of Medicine © Robert M. Youngson 2004, 2005
tam·pon·ade
, tamponage (tam'pŏ-nād', -nazh')1. Pathologic compression of an organ.
2. Act of inserting a tampon.
Medical Dictionary for the Dental Professions © Farlex 2012