Stroke
Definition
Description
- more than one-half million people in the United States experience a new or recurrent stroke each year
- stroke is the third leading cause of death in the United States and the leading cause of disability
- stroke kills about 160,000 Americans each year, or almost one out of three stroke victims
- three million Americans are currently permanently disabled from stroke
- in the United States, stroke costs about $30 billion per year in direct costs and loss of productivity
- two-thirds of strokes occur in people over age 65 but they can occur at any age
- strokes affect men more often than women, although women are more likely to die from a stroke
- strokes affect blacks more often than whites, and are more likely to be fatal among blacks
Causes and symptoms
Causes
Risk factors
- Age and sex. The risk of stroke increases with age, doubling for each decade after age 55. Men are more likely to have a stroke than women.
- Heredity. Blacks, Asians, and Hispanics have higher rates of stroke than do whites, related partly to higher blood pressure. People with a family history of stroke are at greater risk.
- Diseases. Stroke risk is increased for people with diabetes, heart disease (especially atrial fibrillation), high blood pressure, prior stroke, or TIA. Risk of stroke increases tenfold for someone with one or more TIAs.
- Other medical conditions. Stroke risk increases with obesity, high blood cholesterol level, or high red blood cell count.
- Hormone replacement therapy. In mid-2003, a large clinical trial called the Women's Health Initiative was halted when researchers discovered several potentially dangerous effects of combined hormone replacement therapy on postmenopausal women. In addition to increasing the risk of some cancers and dementia, combined estrogen and progesterone therapy increased risk of ischemic stroke by 31% among study participants.
- Lifestyle choices. Stroke risk increases with cigarette smoking (especially if combined with the use of oral contraceptives), low level of physical activity, alcohol consumption above two drinks per day, or use of cocaine or intravenous drugs.
Symptoms
- blurring or decreased vision in one or both eyes
- severe headache, often described as "the worst headache of my life"
- weakness, numbness, or paralysis of the face, arm, or leg, usually confined to one side of the body
- dizziness, loss of balance or coordination, especially when combined with other symptoms
Diagnosis
Treatment
Emergency treatment
Rehabilitation
Prognosis
Prevention
- quitting smoking
- controlling blood pressure
- getting regular exercise
- keeping body weight down
- avoiding excessive alcohol consumption
- getting regular checkups and following the doctor's advice regarding diet and medicines, particularly hormone replacement therapy.
Resources
Periodicals
Organizations
Key terms
stroke
[strōk]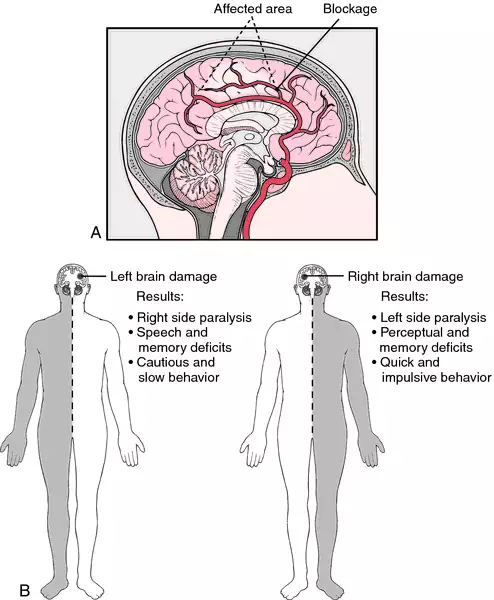
stroke
(strōk), [MIM*601367]See also: stroking. Synonym(s): apoplexy, brain attack
See also: stroking.
See also: stroking.
See also: stroking.
An acute neurologic deficit resulting from circulatory impairment that resolves within 24 hours is called a transient ischemic attack (TIA); most TIAs last only 15-20 minutes. In contrast, a stroke involves irreversible brain damage, the type and severity of symptoms depending on the location and extent of brain tissue whose circulation has been compromised. The outcome of a stroke varies from minimal impairment to rapid onset of coma followed quickly by death. Stroke ranks third as a cause of death in adults in the U.S., after ischemic heart disease and cancer. About 600,000 people a year experience strokes in this country, of which about one fourth are fatal. At any given time the population includes about 3 million stroke survivors. Stroke costs the U.S. national economy more than $40 billion a year. The incidence of stroke has gradually declined during the past generation. Risk factors for stroke include hypertension, valvular heart disease or the presence of a prosthetic valve, atrial fibrillation, left ventricular dysfunction, hyperlipidemia, diabetes mellitus, cigarette smoking, obstructive sleep apnea, a history of previous stroke or TIA, and a family history of stroke. In addition, prolonged estrogen replacement therapy, elevation of plasma homocysteine, low circulating levels of folic acid and pyridoxine (vitamin B6), periodontal disease, and chronic bronchitis are all independent risk factors. Ischemic stroke, which accounts for about 85% of all strokes, is generally caused by atherothrombosis or embolism of a major cerebral artery. Less common causes of ischemic stroke include nonatheromatous vascular disease and coagulation disorders. Severe, acute ischemia in nerve tissue triggers cellular changes (calcium influx, protease activation) that can swiftly cause irreversible damage (infarction). Around the infarct zone lies a so-called penumbra of ischemic, electrically silent tissue that may be salvageable by prompt reperfusion. The mortality of ischemic stroke is 15-30% within the first 30 days. Hemorrhagic stroke, which makes up the other 15%, has a graver prognosis, with a 30-day mortality rate of 40-80%. Carriers of either the e2 or e4 allele of the apolipoprotein E (APOE) gene have an elevated risk of intracerebral hemorrhage. About 30% of ischemic infarcts, including most of those with severe impairment of cerebral blood flow and extensive tissue death, eventually develop a hemorrhagic component. The diagnostic evaluation of the patient with stroke includes history, physical examination, hematologic studies with coagulation profile, blood chemistries, electrocardiogram, and imaging studies. Although cranial CT without contrast enhancement is the procedure of choice to distinguish ischemic from hemorrhagic stroke and to identify subarachnoid hemorrhage, MRI is a more sensitive indicator of parenchymal hemorrhage as well as of early ischemia and infarction, and is more useful in assessing the brainstem and cerebellum and in identifying underlying nonvascular lesions. About 20% of people initially thought to have had a stroke prove to have some other disorder, and as many as 20% of strokes are missed on initial evaluation by emergency department physicians. Early and aggressive treatment is crucial in limiting damage to brain tissue and achieving an optimal outcome. In ischemic stroke, intravenous administration of tissue plasminogen activator (TPA) within the first 3 hours, with the purpose of dissolving an obstructing thrombus, has been shown to improve overall outcome at 90 days. Limiting factors in the use of thrombolytic therapy are the need to rule out hemorrhagic stroke (sometimes difficult with available imaging methods) and the fact that the therapy itself may induce hemorrhage. Intravenous thrombolytic agents other than TPA are not only less effective but also more likely to cause hemorrhage. During the acute phase of a stroke, respiratory and circulatory support and attention to fluid and electrolyte balance and nutrition are vitally important. Hypothermia and intravenous administration of heparin and magnesium also improve outcome in selected cases. Long-term consequences may depend on the aggressiveness and persistence of physical therapy and rehabilitation. About 40% of stroke victims develop depression, a complication that aggravates cognitive impairment and delays recovery. Effective measures for the prevention of stroke include aggressive management of hypertension (relative risk reduction, 30-50%), hyperlipidemia (30-40%), and diabetes mellitus; cessation of smoking; and chemoprophylaxis in patients at high risk. Administration of aspirin (acetylsalicylic acid) prophylactically inhibits platelet aggregation by suppressing thromboxane A2. Metaanalysis of randomized controlled trials involving a total of more than 50,000 people indicated that low-dose aspirin (81-325 mg/day) reduces the risk of ischemic stroke by 39 events per 10,000 people but increases the risk of hemorrhagic stroke by 12 events per 10,000 people. Other studies suggest that aspirin at higher dosage (1.3 g/day in divided doses) protects men but not women from ischemic stroke because in women aspirin also suppresses prostacyclin, a natural inhibitor of platelet aggregation. Prophylaxis with other antiplatelet agents (clopidogrel, ticlopidine) is equally effective in men and women and at least as protective as aspirin. In nonvalvular atrial fibrillation, warfarin prophylaxis reduces stroke risk by two thirds. In people with carotid artery stenosis of more than 70%, carotid endarterectomy clearly reduces the risk of stroke. The National Stroke Association has recommended adoption of the term brain attack for stroke, by analogy with the familiar heart attack, to emphasize to the public both the location of the lesion and the urgency of the need for assessment and treatment. see also tissue plasminogen activator.
stroke
(strōk)stroke
A clinical syndrome consisting of rapidly developing clinical signs of focal (at times global) disturbance of cerebral function, lasting more than 24 hours or leading to death, with no apparent cause other than that of vascular origin.stroke
Cerebrovascular accident Neurology A sudden focal neurologic defect lasting > 24 hrs, which is characterized by abrupt loss of consciousness due to either hemorrhage or vascular occlusion of cerebral blood vessels, leading to immediate paralysis, weakness, speech defects; a sudden onset of neurologic deficit of vascular origin; strokes are a leading cause of disability in developed countries–500,000 new victims/yr, US, 20-30% of whom are left with severe residua; strokes are the 3rd leading cause of death–20-30% early mortality; the incidence of stroke rises dramatically with age; the risk doubles every decade after age 35 Statistics, mortality < 80 deaths/105: Whites in US–especially in the midwest, Australia, New Zealand, northern Europe, Egypt; >130 deaths/105: Black US–especially in south, Russia, mainland China, former Eastern Blocks, Argentina Clinical Paralysis, weakness, sensory loss, speech defects Etiology ASHD, dissection or stenosis of carotid artery, cocaine, embolism, HTN, fibromuscular dysplasia, syphilis Treatment Warfarin ↓ risk of stroke in Pts with A Fib or previous MI; in poor candidates for warfarin therapy, aspirin–which is less protective ± ticlopidine; carotid endarterectomy–useful if 70+% stenosis; CE's role in asymptomatic Pts is uncertain; dipyridamole and sulfinpyrazone are useless. See Completed stroke, Delayed stroke, Embolic stroke, Hemorrhagic stroke, Recent completed small stroke, Sunstroke, Working stroke.stroke
(strōk)See also: cerebrovascular accident
See also: stroking
Synonym(s): apoplexy.
stroke
The effect of acute deprivation of blood to a part of the brain by narrowing or obstruction of an artery, usually by thrombosis (80 %), or of damage to the brain substance from bleeding into it (CEREBRAL HAEMORRHAGE) (15%). Subarachnoid haemorrhage is the cause in 5%. The results of such damage are most obvious if they involve the nerve tracts concerned with movement, sensation, speech and vision. These are situated close together, in the internal capsule of the brain, and are often involved together. There may be paralysis and loss of sensation down one side of the body or of one side of the face, loss of corresponding halves of the fields of vision, a range of speech disturbances or various disorders of comprehension or expression. In most cases a degree of recovery, sometimes considerable, may be expected. Haemorrhage into the brainstem, where the centres for the control of the vital functions of breathing and heart-beat are situated, is the most immediately dangerous to life. Diagnosis of the type of stroke is important and this requires neuroimaging of the brain.ophthalmodynamometer (ODM)
stroke
(strōk) [MIM*601367]Patient discussion about stroke
Q. Stroke My granny got stroke. Now she is in the hospital, but she doesn't identify me or my mother. When I asked her what are the season now - she answers that it's winter now. I don't know how to help her. What I have to prepare for?
Q. Migraine stroke Hi, I'm 58 years-old male and I have migraines with aura since age 14. Two weeks ago, I felt weakness in the left side of my body, and at the hospital the doctors told me I had a stroke. I underwent several tests, but they still don't know the cause for the stroke (my lab tests are normal; I don't have diabetes or hypertension). My neurologist said that although it's very rare, he thinks that my stroke was caused by my migraine. I tried to find information about it, but couldn't find much – do you know where I can get some more info? Thanks!
Q. What Are the Risk Factors for Developing Stroke? My father had a stroke recently, at the age of 73. What are the risk factors for developing this?
1) smoking
2) excessive alcohol intake
3) uncontrolled high blood pressure
4) high cholesterol
5) overweight/unhealthy diet
6) illegal drugs/abuse of Rx drugs
7) known or unknown heart problems
8) diabetes
9) known or unknown vascular brain defects - aneurysm, etc.
10)family history of stroke